@crippshallassociation Oliver Cujic, a final year medical student, was supported by The Cripps Hall Trust to complete a medical elective at Dr. Jeyasekharan Medical Trust – College of Nursing and Allied Health Sciences in Nagercoil, Tamil Nadu, India. https://crippshalltrust.org.uk/2025/06/dr-jeyasekharan-medical-trust-nagercoil-india-oliver-cujic-2025/ #travel#scholarship #weareuofn #crippshall #nottinghamuniversity ♬ original sound - Cripps Hall Association
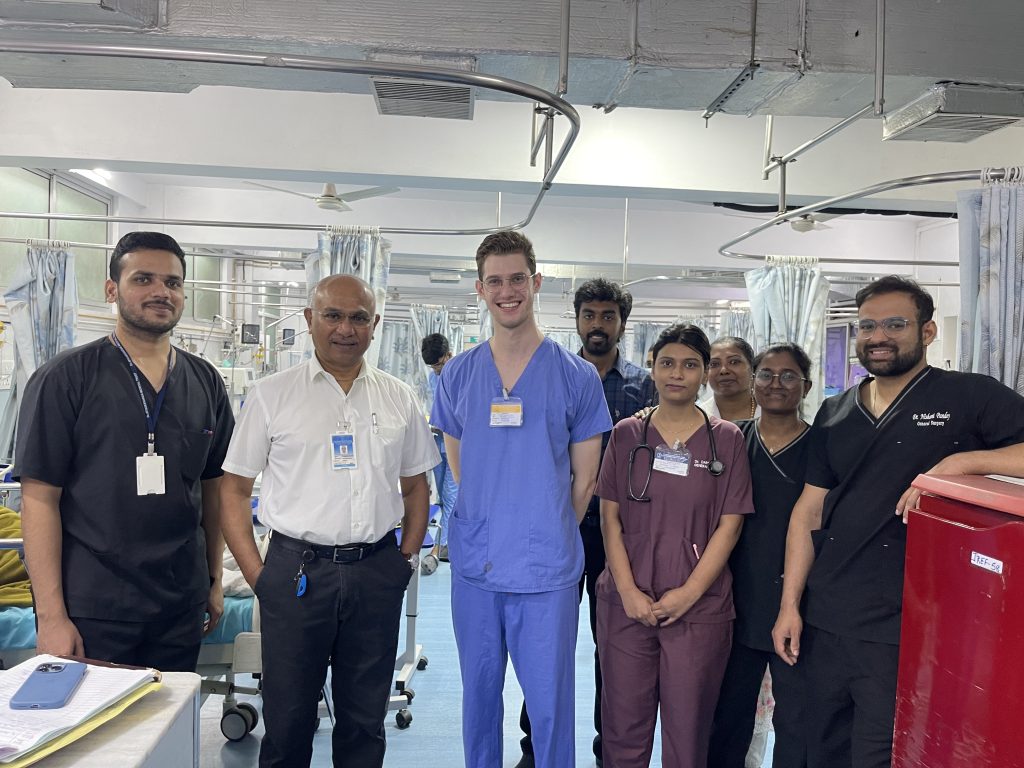
I recently travelled to India, where I had the incredible opportunity to complete my medical elective at Dr. Jeyasekharan Medical Trust – College of Nursing and Allied Health Sciences in Tamil Nadu. My placement was based in the General Surgery department, a specialty I am interested in and one that I hope to pursue as a career. This elective provided a unique and invaluable insight into the Indian healthcare system. I gained extensive clinical exposure, developed a better understanding of the structure of medical education in India, and immersed myself in the rich culture and customs of Tamil Nadu.
The hospital is a well-established, multidisciplinary institution situated in Nagercoil, in the southernmost district of the Indian mainland. It runs both a private hospital and an affiliated nursing and allied health sciences college. The combination of clinical and academic environments made it an ideal setting for a medical elective with many interesting patients and trainee doctors to learn from.
During my time there, I attended daily ward rounds, outpatient clinics, and operating theatre sessions. I rotated through the general surgical ward, the surgical intensive care unit (SICU), and the post-operative recovery unit. Each of these placements offered something different and contributed to a broader understanding of surgical care from admission through to recovery and discharge. The clinical staff were highly welcoming and often made time to explain procedures, diagnoses, and local protocols.
In addition to my clinical attachment, I was fortunate to participate in a number of academic activities. I attended the hospital’s weekly journal club, where current research papers were discussed and critically appraised. These sessions were an excellent opportunity to engage with evidence-based practice and understand the evolving nature of surgical management. I also sat in on a postgraduate surgical lecture at Kanyakumari Government Medical College, which covered real-world clinical scenarios where the consultant grilled the junior doctors and cross examined their clinical decision making.
Clinically, I was exposed to a wide variety of diseases—some more common in South India and others similar to those encountered in the UK. I observed several cases of tropical diseases such as typhoid fever, tuberculosis and hepatitis which are rarely seen in clinical practice in the UK. I also saw a growing number of conditions associated with changing lifestyles, including diverticulosis and inflammatory bowel disease. These ‘Western’ conditions appear to be on the rise in India, which the doctors attribute to urbanisation and dietary shifts. It was interesting to see how lifestyle factors were discussed during consultations and how patients were counselled differently compared to what I’ve seen in the UK.
Another striking observation was the presentation of diseases at more advanced stages than we would typically encounter in the UK. Delayed access to care—often due to financial constraints, distance from hospitals, or cultural hesitancy—meant that many patients presented with more progressed pathology. For instance, I saw a patient with a very enlarged thyroid gland due to follicular hyperplasia. In the UK this would have been treated sooner which would have made the operation easier, quicker and safer. These delays inevitably complicate treatment and can lead to worse outcomes.
One particularly memorable and sobering case involved a young woman who had sustained grievous bodily harm. She had multiple stab wounds to her face, neck, and torso. The knife had remained lodged in her neck, and she was taken to emergency theatre late at night for surgical exploration and removal. Despite the tragic circumstances, it provided a good learning opportunity and insight into trauma management, rapid surgical assessment, and teamwork under high-pressure conditions.
Other notable cases included several patients with Fournier’s gangrene—a severe form of flesh eating bacteria (necrotising fasciitis) that affects the perineum and genital area. These cases often required emergency debridement, intensive care, and in some cases, reconstructive procedures. In one particularly severe instance, I observed a patient undergo circumcision and extensive perineal reconstruction following debridement. The management of such aggressive infections demonstrated the need for timely intervention, multidisciplinary teamwork, and post-operative vigilance.
In the operating theatres, I had the opportunity to observe a variety of procedures, including a total thyroidectomy for follicular hyperplasia, a percutaneous nephrolithotomy (PCNL) for a large staghorn calculus, laparoscopic appendicectomy, and a lower segment caesarean section. Several of these operations I had seen performed in the UK, so I found it fascinating to compare the techniques, instruments used, and approaches to anaesthesia.
Experiencing healthcare in a setting so different from the NHS was eye-opening. While my placement was primarily in a private hospital with relatively good access to resources, I also had the opportunity to visit the nearby Kanyakumari Government Medical College. There, I was given a tour of the surgical wards and operating theatres. One aspect that stood out was that multiple patients were being operated on simultaneously in the same theatre. This practice is not seen in the UK due to infection control policies and patient confidentiality; however, I was informed that such measures are often a necessity due to a shortage of anaesthetists. This allows one anaesthetist to manage multiple patients at once and maximises how many operations can be performed in a given time.
These differences in practice gave me a broader understanding of the challenges faced by low- and middle-income countries in delivering surgical care. I gained a deeper appreciation of the ways in which healthcare professionals adapt to limitations while striving to maintain patient safety and quality of care. It also made me reflect on the enormous value of the NHS and the privilege of universal healthcare, something that can often be taken for granted in the current climate of issues facing the NHS.
Outside of the hospital, my experience of Tamil Nadu was just as enriching. I was warmly welcomed by the staff and their families, who went out of their way to help me experience local life. I was invited to traditional meals, market visits, and weekend trips to the Western Ghats mountains. I tried a wide range of regional dishes, such as dosa and sambar, and even learned to eat with my hands in the traditional South Indian way. These cultural experiences gave me a more holistic understanding of the region and its people, and deepened my appreciation for how culture influences attitudes to health and illness.
This elective has undoubtedly been one of the most formative experiences of my medical training. I am confident that this experience will enhance my future medical practice, particularly when working with patients of South Asian heritage in the UK. Understanding the cultural context of illness, the barriers to healthcare access, and the differences in disease presentation will help me to deliver more empathetic, informed, and individualised care.
ACKNOWLEDGEMENTS
I would like to express my sincere gratitude to all the staff at Dr. Jeyasekharan Medical Trust, especially Dr. Sabu Jeyasekharan, Dr. Devaprasath Jeyasekharan, and Dr. Renu Devaprasath, for their warm hospitality, kindness, and generosity. Their support extended far beyond the hospital and allowed me to fully immerse myself in Tamilian life.
Finally, I am incredibly thankful to The Cripps Hall Trust for awarding me the Harry Lucas Travel Scholarship. Without their financial support, this elective would not have been possible, and I am truly grateful for this opportunity.
Oliver Cujic,
Medical Student, The University of Nottingham.
(April 2025)